Complications and other problems from Gastric Banding or Lap Band Surgery
Unfortunately every surgical procedure has potential complications that must be understood prior to committing to surgery.
Complications around the time of surgery are uncommon with band surgery. Mostly the surgery is uneventful and patients go home after one night in hospital or even the same day of surgery in some cases. It is possible to damage the stomach or oesophagus whilst placing the band however this risk is probably in the order of approximately 1/500.
Many of the problems, complications or issues with the band actually happen some time down the track after initial surgery.
Note that if a gastric band has failed to produce good results or is causing problems my preference is conversion to gastric bypass surgery if further weight loss surgery is desired. This is an effective and well studied alternative although complication rates are higher than having a straight forward bypass up front. Sleeve gastrectomy is also possible after banding surgery. Either surgery requires re-operating through the scarred up and distorted area at the top of the stomach where the band used to be.
Access Port Related Problems
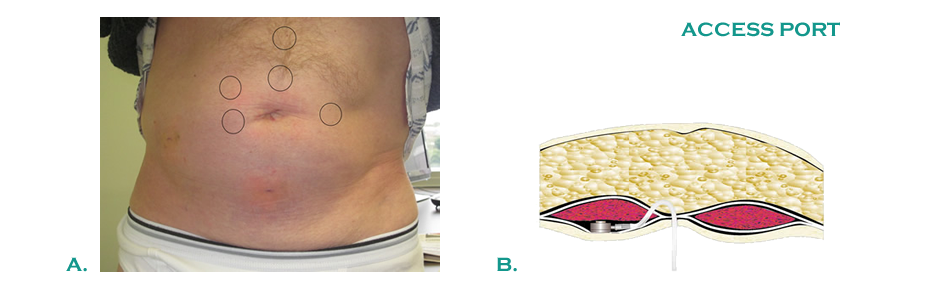
A.: Some of the more commonly used positions for the gastric band access port
B : This port has been placed underneath the muscle to prevent excessive protrusion
1. Infection
This may occur shortly after initial surgery or down the track. If it occurs shortly after surgery it is probably related to wound infection or infection of a haematoma or blood collection around the port. If it occurs spontaneously down the track it may be related to erosion of the band into the stomach (see below).
Key Point: Spontaneous infection of the access port some time after surgery is often associated with band erosion
2. Flipped Port, Migrated Port
This is suspected when attempts to adjust the port with a needle are excessively difficult or impossible. An xray may confirm the abnormal position of the port. A flipped or migrated port can occur if the locking mechanism does not engage properly at the time of surgery or the sutures do not hold. A flipped or migrated port can be easily fixed with a simple procedure under general anesthetic.
3. Skin Erosion
This can occur when the skin stretches tightly across the access port, usually after a period of weight loss thins out the subcutaneous fat layer between the skin and the port. The port will need to be moved, possibly underneath the abdominal muscle layers to prevent further problems
4. Leak of Fluid
Fluid can leak from the system, either from the port itself, the connection from the tubing to the port, the tubing itself or rarely from the band itself. Multiple attempts to access a difficult port with a needle can sometimes injure the tubing. The tubing itself can kink and erode through with time if poorly placed. A leak of fluid is suspected when multiple band fills fail to induce satiety and restriction. The port is then re-accessed to find that all the fluid is gone. A special xray can help localise the site of the leak but these are often negative studies. The leak can usually be localised with a small operation and the access port revised or replaced.
5. Port site hernia
A weakness in the muscle layer around the port may sometimes occur, necessitating repair of the “hernia”. This is usually possible to do without disturbing the current port position.
Band Related Problem
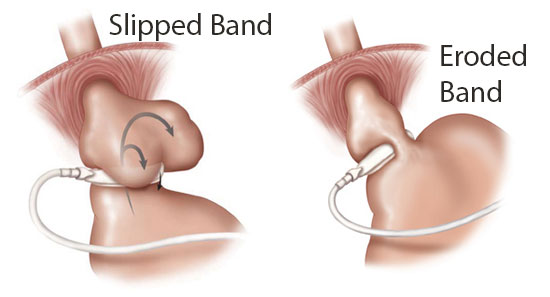
1. Slipped band (5%)
The band is originally placed around the top of the stomach. Despite attempts to fix the band in place with sutures, bands can sometimes slip down the stomach to an abnormally low position. Another way to look at it is that the lower stomach is forced up through the band due to pressure. It is thought that protracted vomiting with the band because of poor dietary choices or excessive restriction may predispose to slippage by constant increases in abdominal pressure.
The band is not designed to sit around the middle of the stomach and it is common for “obstructing” symptoms to occur. This results in excessive vomiting, acid reflux and food intolerance. In the worst case scenario the stomach can be completely obstructed with no passage of fluid or food possible. This is a potentially dangerous situation in which urgent medical care should be sought. It is possible for the band to cut off the blood supply to the entrapped stomach and for this part of the stomach to die. This is a life-threatening emergency if this occurs.
The first step in managing a slipped band is to remove all the fluid to reduce obstruction.
Thereafter the options are as follows:
- Remove the band completely
- Re-position the band surgically back into its correct position
- Remove the band and convert to another weight loss operation such as gastric bypass
Key Point: If you are unable to drink fluids with a gastric band in place you should seek immediate specialist attention to avoid death of the stomach if your band has slipped
Unstable Band?
Recently we have noticed a number of patients who appear to have mobile or dislocating bands. This means that the band is sometimes in the correct location and sometimes moves to a "slipped" position which will cause food intolerance and vomiting. The amount of fluid inside the band appears to be the most important factor which governs whether the band resides in the slipped position or is properly located. In some patients who have persistent difficulties achieving the correct amount of band fill to allow portion control and control hunger and avoid excessive vomiting we will investigate for this phenomenon. Investigation of the unstable band is best done by gastroscopy where we insert a flexible fibre-optic telescope into the pouch above the band and observe for excessive movement upon maximal filling and deflation of the band. Another way of diagnosing the problem is with a special barium contrast swallow where bread soaked in a substance which is visible on x-rays is swallowed and monitored on its journey through the stomach. The high pressures caused by the body moving the bread through the band may elicit abnormal motility of the band in some cases.
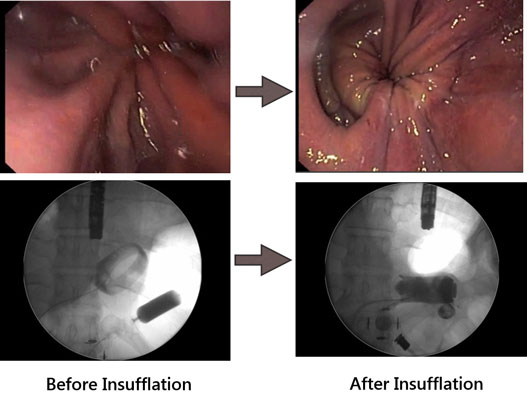
Above: Gastroscopy images demonstrating unstable band. On the left is a normal sized gastric pouch above a band. The band is filled with fluid and air insufflated into the pouch via the scope. A dilated eccentric pouch has formed consistent with a slipped band.
Below: Xray pictures of the band during the described maneouver. The band has moved from the normal, angled position (left) to the horizontal or slipped position (right).
2. Band Erosion (1%)
This is an uncommon complication whereby the silicone ring of the band actually passes through the wall of the stomach so that it resides partially inside the stomach rather than sitting around it. This automatically means that the band is infected and occasionally this infection will make its way to the access port. Restriction is often lost in this circumstance and the patient gains weight. Abdominal pain is often experienced.
The treatment of erosion is to remove the band. This is usually done laparoscopically although in some circumstances it may be done from within the stomach with a special band-cutting device. The upper stomach is usually in fairly poor condition after erosions and needs a period of healing to occur before any further surgery can be contemplated. It is possible to perform further weight loss surgery after erosions have occurred but this needs to be carefully discussed with your surgeon. Replacing bands after erosions leads to high re-erosion rates. Other procedures such as gastric bypass or sleeve gastrectomy may be possible alternatives to re-banding.
3. Pouch dilatation (occasional)
The small stomach pouch above the band can stretch with time leading to an enlarged pouch above the band. This is detrimental as it gives poor restriction of food volume and leads to vomiting and acid reflux in some cases. Pouch dilatation can be diagnosed on a barium swallow study.
The first step in treating pouch dilatation is usually to release the fluid from the band for a period of time. This may give the stomach a chance to relax and recover. If the problem persists after this trial, re-operation with re-positioning of the band is usually possible. Another consideration is to convert the band to another weight loss procedure such as gastric bypass.
4. Oesophageal dilatation (occasional)
The oesophagus (gullet, or food-pipe that transmits food from the mouth to the stomach) has to work hard pushing food through the band. In some patients, particularly if the band is tight or dietary habits are poor, it starts to “burn out” a little from the effort and may lose strength. When an xray is done, the oesophagus appears to have expanded, or dilated from the excessive efforts over the years. In this case it is best to give the oesophagus a period of rest by releasing the band completely for awhile. With time, oesophageal function should improve if the outlet is released.
5. Band intolerance
Some patients have difficulty with the band without any identifiable technical issue. These patients get frequent vomiting and reflux with the band and find eating good foods difficult much of the time. Multiple attempts at adjusting the fluid levels within the band fail to find a place which is comfortable and effective for the patients.
There is no easy solution for band intolerance if a technical problem cannot be identified. Occasionally on surgical exploration a hiatus hernia (weakness of the diaphragm) may be repaired and the band re-positioned which might lead to successful resolution in some cases. In other cases the band may simply need to be removed and consideration of revision to bypass or sleeve may be undertaken.
6. Hiatus hernia
It is generally accepted that a hiatus hernia (weakness of the diaphragm muscle) if present should be repaired when the band is initially placed. Occasionally a hiatus hernia may occur after a band is placed or have been missed at the original procedure. If there are debilitating symptoms such as excessive vomiting, reflux or food intolerance it is likely that re-operation with repair of the hiatus hernia and re-positioning of the band may ameliorate these symptoms
7. Tubing problem
Part of the tubing connecting the band balloon to the access port resides inside the abdomen itself. There are rare reports around the world of the tubing causing mischief inside the abdomen, such as entrapment of a loop of bowel within itself. These problems can be serious but are fortunately rare.
8. Leaking band (rare)
The band will need to be replaced if the balloon is leaking.
9. Infected band (rare)
The band will need to be removed with possible replacement at a later date.
When no other solution is possible for a failing gastric band and further weight loss surgery is desired, my preference is conversion to gastric bypass surgery